Suturing is a critical step in oral surgery—not just a means of closing wounds, but a biological strategy for promoting proper healing, maintaining flap stability, minimizing bleeding, and preventing infection.
The effectiveness of suturing directly influences postoperative outcomes, especially in procedures such as third molar extractions, implant surgeries, periodontal regeneration, and soft tissue grafts.
Over the past five years, advances in surgical materials and minimally invasive techniques have led to a reevaluation of suturing methods.
The selection of suture type and technique is no longer based solely on the surgeon's preference, but rather on a multifactorial analysis: wound tension, anatomical site, healing time, risk of contamination, and esthetic expectations—particularly in anterior regions.
Additionally, innovations in suture materials—such as monofilament synthetic threads with low bacterial adherence—have shifted clinical preferences toward methods that ensure tissue integrity with minimal inflammation.
Let's explore the most widely used suturing techniques in oral surgery today, grounded in recent scientific evidence.
Main Suturing Techniques in Oral Surgery
🔹 1. Simple Interrupted Suture
✔ Indications: Basic flap closure after extractions or minor procedures.
✔ Advantages: Individual control of tension at each point; easy to remove; low risk if one stitch fails.
✔ Limitation: Time-consuming compared to continuous techniques.
🔹 2. Continuous Suture
✔ Indications: Linear or long incisions.
✔ Advantages: Even tension distribution; faster placement.
✔ Disadvantage: If one segment fails, the entire suture may loosen.
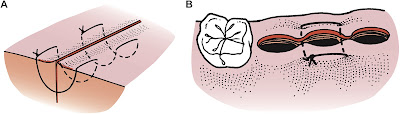
🔹 3. Mattress Suture (Horizontal and Vertical)
✔ Horizontal: Used in low-tension wounds; aids in hemostasis.
✔ Vertical: Anchors deep and superficial layers; useful in mobile tissues.
✔ Commonly used in: Periodontal and mucogingival surgeries.
🔹 4. Figure-of-Eight Suture
✔ Indications: Stabilizing extraction sockets, especially third molars.
✔ Advantages: Protects blood clot and supports wound edges.
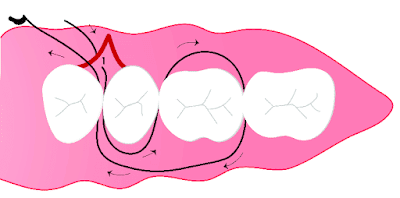
🔹 5. Sling Suture
✔ Indications: Securing grafts or tissues around teeth or implants.
✔ Advantages: Allows precise control over gingival margins.
✔ Used in: Mucogingival and peri-implant procedures.
🔹 6. Periosteal Sutures
✔ Indications: Fixation of membranes or tissue grafts over bony ridges.
✔ Comment: Advanced technique requiring surgical expertise; offers strong anchorage.
Clinical Criteria for Technique Selection
Clinical Scenario / Recommended Technique
✔ High wound tension: Vertical mattress suture
✔ Esthetic zones: Continuous with fine monofilament
✔ Hemostasis needed: Horizontal mattress or figure-of-eight
✔ Implant surgery: Sling suture with PTFE or polypropylene
✔ Ridge augmentation or graft fixation: Periosteal or combination techniques
Proper technique also includes
✔ Avoiding excessive tension to prevent ischemia.
✔ Ensuring moist but uncontaminated wound environments.
✔ Choosing sutures with high tensile strength and low tissue reactivity in moist oral conditions.
Scientific Trends (2019–2024)
✔ Increased use of synthetic monofilament sutures (PDS, PTFE, Polypropylene) due to lower bacterial colonization.
✔ Combination techniques (e.g., sling + interrupted) for better soft tissue stabilization.
✔ Exploration of barbed sutures (knotless) in oral surgery, still under investigation.
✔ Technique personalization based on individual tissue healing response.
📚 Recommended Reading
- Journal of Oral and Maxillofacial Surgery. August 2015 • Volume 73 • Supplement 1. GUIDE TO SUTURING with Sections on Diagnosing Oral Lesions and Post-Operative Medications